TSC teachers’ SHA medical scheme (POMSF): Full details & benefits
Table of Contents Show
PRESENTATION ON TEACHERS MEDICAL COVER UNDER PUBLIC OFFICERS MEDICAL COVER (POMSF)
BRIEF ON TSC MANDATE
The Teachers Service Commission, TSC, is an independent constitutional commission established under Article 237(1) with the mandate to: register trained teachers, recruit and employee registered teachers, assigned teachers employed by the commission for the service in any public school or institution, promote and transfer teachers, exercising disciplinary control over teachers, terminate the employment of teachers, review the standard of education and training of persons entering the teaching service, review the demand for and the supply of teachers and advice the National Government on matters relating to the teaching profession.
BACKGROUND ON THE TEACHER’S MEDICAL COVER
The Teachers Medical Cover was set up in July 2015 under Minnet as the administrator by the Commission to replace the medical allowance. Over time the Commission has improved on the management of the cover by:
- Setting up a Contract Implementation team;
- Devolving the monitoring of the contract implementation at various levels i.e counties; and
- Progressively reviewed the cover scope over time to align with the needs of teachers.
CHALLENGES OVER THE PERIOD OF IMPLEMENTATION OF THE MEDICAL COVER
Despite the continuous improvement the following challenges persisted:
- Limited empaneled hospitals across the country;
- Insurance model;
- Rejection of admission requests forcing teachers to use their own resources;
- Lengthy procedures in Pre-authorization or approval for admissions and discharges;
- Inadequate specialists in most facilities, especially outpatient services;
- Inadequate supply of original quality drugs;
- Poor management of Chronic conditions;
- Few optical and dental care providers empaneled;
- Restricted cover for dependants (moreso for teachers with more dependants than the maximum provided by the employer);
- Lengthy onboarding criteria; and
- One fit benefit structure.
COMMISSION’S ACTION TO MITIGATE THE CHALLENGES
Following enactment of the regulations of the POMSF the Commission intends to engage the Social Health Authority to manage the teachers Medical Cover with the existing covers limits under the Public Officers Medical Scheme Fund.
ACTIONS TO MITIGATE CHALLENGES
| CHALLENGE | MITIGATION MEASURE | |
| 1. | Limited empaneled hospitals across the country (816) | SHA will now give 9,016 hospitals across the country. (these include, public, private and faith based hospitals) |
| 2. | Rejection of admission requests are now forcing teachers to use their own resources | The admission process has now been fully automated with zero human interface. The teacher will be required to utilize his/her limits responsibly to cover the year. |
| 3. | Insurance model (run on a business model) | The proposed model will be a fee for service model |
| 4. | Lengthy procedures in Pre-authorization or approval for admissions and discharges | This process has been fully automated (no human interface) |
| 5. | Inadequate specialists in most facilities, especially outpatient services | This has been addressed by the increased number of facilities |
| 6. | Inadequate supply of original quality drugs | This is now a fee for service subject to a teachers limit rather than insurance |
| 7. | Management of Chronic conditions | In addition to the benefits (inpatient, outpatient and overseas) under POMSF which takes care of chronic/existing conditions SHA will now bring onboard two other benefits i.e SHIF(Social Health Insurance Fund) and ECCIF(Emergency, Chronic And Critical Illness Fund) |
| 8. | Few optical and dental care providers empaneled | Most of the empannelled hospitals have their own dental and optical care services in addition to accredited specialists. |
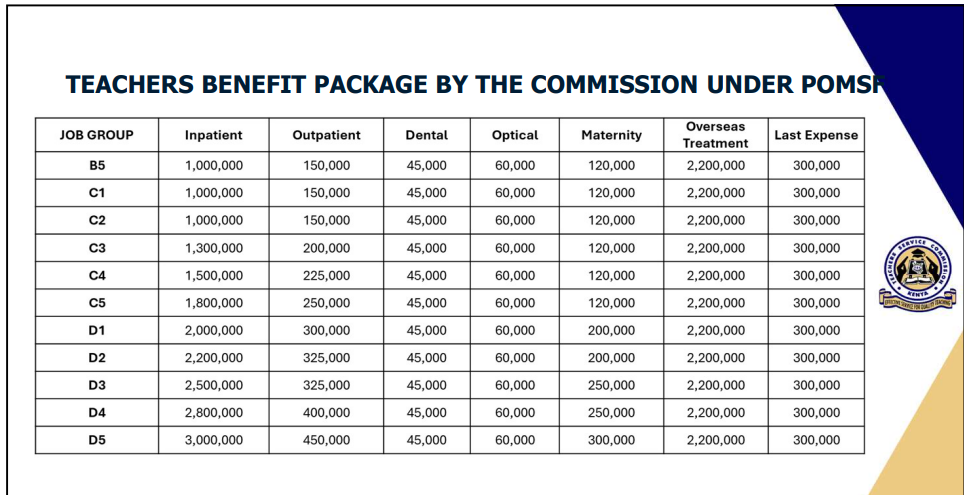
TEACHERS BENEFIT PACKAGE BY THE COMMISSION UNDER POMSF
SCOPE OF COVER
1. Principal Member
2. Declared spouse
3. Declared children (up to 5 children):
• Up to 21 years of age
• A maximum of (25) years of age if wholly dependent on the principal member and enrolled in full-time post-secondary education;
• A child with disability who is wholly dependent on the principal member – in this case there shall be no age limit for coverage of a person with disability declared as a dependent of the principal member
• Additional children above the five covered can be included at an additional premium paid by the principal member.
REGISTRATION PLATFORMS & PROCESSES (SELF)
Web Self-registration
- On your web browser, open the SHA website- https://sha.go.ke/
- click on register and start the registration process.
USSD Self-registration
- Dial *147# on your mobile device then proceed to accept the SHA terms and conditions.
Assisted Enrolment
- It is assisted registration done in our SHA branches, Huduma Centres and TSC County and Subcounty offices
Registration of Teenage & Underage Mothers
Registration now possible for teenage mothers at SHA branches, Huduma Centres and TSC County and Subcounty offices.
REGISTRATION & UPDATING OF BENEFICIARIES
- Spouse-ID of spouse and proof of marriage
- Child-Birth notification/Certificate
- Adopted Child-Adoption Order
A child for who the contributor is a Guardian-Will, Deed or court order or other document recognized under the Children’s Act
- Person with Disability-ID & Certificate of Registration from National Council for Persons with Disabilities
- Persons under lawful custody-Prison admission number or remand identification number of copy of ID
- Child in conflict with the law-admission number of the children’s remand home, rehabilitation institution or borstal institution or Child’s birth certificate
CHANGE OF SPOUSE
- A 30-day waiting period applies when a member changes their declared spouse for the first time before the new spouse becomes eligible for services.
- For any subsequent spouse change, a 6-month waiting period applies before eligibility for services
- In case the change is due to death of a spouse, the waiting period does not apply.
HOW TO ACCESS MEDICAL BENEFITS
Accessing Outpatient services
i. All scheme beneficiaries shall access outpatient services on fee for service within their limits which are on family shared basis.
Requirements at the Healthcare Provider
A copy of the National Identification Card with Biometric and/or OTP verification.
Accessing Inpatient Services
All scheme beneficiaries shall access inpatient services on fee for service within their limits which are on family shared basis.
Documents required at point of service
i. A copy of the spouse’s ID.
ii. Copy of birth certificate for a child or copy of birth notification for child below six (6) months or copy of adoption certificate.
iii. A copy of registration Certificate with the National Council for Persons with Disability
iv. A letter of proof that the child is enrolled in a full-time learning institution for children above 21 years will be required.
TEACHERS BENEFIT PACKAGE BY THE COMMISSION UNDER POMSF
Comprehensive Benefit Package Summary
1. Outpatient & Inpatient Cover
2. Maternity package
3. Dental and Optical
4. Radiology services
5. Renal Dialysis
6. Oversees treatment
7. Annual medical checkup
8. Chronic Illness
9.Tests for donors
10. Evacuation services
11. Drug and substance abuse rehabilitation
SHA BENEFITS PACKAGE DETAILS
Outpatient Cover
Cover includes; Consultation with a General Practitioner & Specialist, basic laboratory investigations, drugs & dispensation, health education, wellness and counselling,
Physiotherapy services and the following vaccines; KEPI vaccines, Rota virus vaccine, Anti- rabies and Anti-snake venom.
Inpatient Cover
Cover includes hospital stay with health care diagnosis, consultation, accommodation/bed charges, nursing care, diagnostic laboratory tests, radiology examinations, physician’s, surgeon’s, anaesthetist’s, physiotherapist’s fees, operating theatre charges, specialist consultations or visits, prescribed medications and dressings.
Maternity & Reproductive Health
- Antenatal care, delivery through both Normal Delivery or Caesarian Section and Postnatal care.
- Family planning services
- Management of postnatal and neonatal complications within applicable inpatient limits
Surgical Package
Includes all surgical procedures(minor, major and specialized) including transplants with an exception of cosmetic surgeries.
Organ Donor Testing
Pre-test costs for the kidney donor identification up to a maximum of two (2).
Renal Dialysis
It caters for hemodialysis for the needed care plan including Specialists’ reviews, nursing and dialysis services, intra-care and dispensed medications, routine laboratory tests, nutrition, counselling and follow up.
Rehabilitation Package: Drug and Substance Abuse
Includes rehabilitation treatment for persons addicted to harmful or hazardous psychoactive substances.
Radiology Package
Includes ALL diagnostic imaging services e.g. CT-Scan, MRI, Mammography, EEG, ECG
Orthopedic and Other Appliances
Covers devices such as hearing aids, prosthetics, and mobility aids (e.g., crutches, wheelchairs)
Oncology Package
Includes treatment for cancer patients using radiotherapy, chemotherapy, hormonal therapy and immunotherapy.
Dental Package
Covers consultations, orthodontics, root canal treatment, post-root canal crowns, fillings, X-rays, and extractions (including surgical extractions).
Optical Package
Includes cost of consultation with ophthalmologist/optometrist, eye testing, glasses for refractive errors, optical frames and lenses.
Emergency Care
Covers emergency evacuation(road & air) for principal members and dependants to facilities with adequate care, ensuring timely access to critical treatment.
Foreign Treatment
Cover for treatment costs arising from a condition that warrants treatment that is not available in Kenya. Cover includes;
- Treatment cost for patient and organ donor where applicable,
- Cost of travel and accommodation for the patient and one person accompanying the patient,
- Cost of travel and accommodation for medical personnel accompanying a patient on recommendation by the referring Doctor for a period not exceeding two days.
Overseas Treatment
- The process for accessing overseas or foreign treatment is as follows:-
1. Referral letter from the treating doctor.
2. A potential donors must be a registered SHA member
Travel Insurance
Emergency cover is provided for a principal member who is on official duty out of the country for a period not exceeding 6 weeks.
SHA shall provide travel insurance cover on request to a Principal Member travelling outside the country.
The following are the requirements for issuance of travel insurance:
1. Clearance letter from the authorizing officer;
2. Cover letter to SHA from the respective employer;
3. Copy of Bio-Data page of the Passport/ Travel Pass Document;
4. Proof of travelling date.
Last expense
Caters for funeral expenses upon the death of the principal member.
Requirements
- Duly completed claim form
- Copy of burial permit
- Copy of deceased’s ID
Specialized Treatment
• Specialized services will be on referral basis.
• The healthcare provider is required to seek preauthorization for specialized services.
• These services shall be on fee for service basis.
• Services available in SHA Empaneled and Contracted Facilities
Services Covered
- Renal Dialysis & Renal Transplant
- Optical & Dental
- Chronic Illness e.g., Diabetes, Hypertension
- Radiological Tests e.g., MRI & CT Scan
- Oncology
- Orthopaedic Appliances
- Drug and Substance Abuse Rehabilitation
- Overseas Treatment
Annual Medical Checkup
Provides comprehensive annual health assessments for the principal member and spouse including;
- Full history and physical examination
- Blood pressure testing;
- Random or fasting blood sugar testing;
- Cancer screening; Pap Smear and Prostate Specific Antigen (PSA) test
- Electrocardiograph (ECG);
- Lipid Profile
- Stool Analysis
- Urinalysis
- Breast ultrasound or mammogram;
- Liver function test;
- Kidney function test;
- Body Mass Index (BMI) test and nutritional advice.
EXCLUSIONS
• Treatments at non-contracted facilities or unauthorized referrals, to maintain quality and cost control.
• Treatments by chiropractors, acupuncturists, or herbalists, as these are outside the scheme scope.
• Self-prescribed treatments, services, or commodities, to prevent misuse.
• Expenses for non-conventional therapies including weight management drugs, nutritional supplements, stop-smoking aids, or domestic remedies unless prescribed as part of medical treatment.
• Costs from clinical trials or research environments, to focus on proven treatments.
Additional Benefits out of the arrangement
THE FUNDS
- PRIMARY HEALTHCARE FUND
- SOCIAL HEALTH INSURANCE FUND
- EMERGENCY, CHRONIC AND CRITICAL ILLNESS FUND
- PRIMARY HEALTHCARE FUND
- INDIVIDUALS CONTRIBUTE PREMIUMS
- GOVERNMENT FUNDING
- Benefits accessed by all registered members to SHA
- Benefits accessed only by paid-up members
- Accident and Emergency services accessible to all Kenyan residents
PHC Package
• Outpatient – KES 900 per annum per beneficiary
• Optical Services – Limit of KES 1,000 per annum (children < 18 years)
SHIF PACKAGE
Inpatient
KES 2,240 – 4,480 per day of admission up to 180 days per household
Maternity
Normal delivery – KES 10,000 • C- section – KES 30,000 • Anti-D Serum – KES 6,000
Oncology
KES 400,000 per member per annum
Renal Care
• Renal Dialysis – KES 10,650 upto 2 sessions per week
• Peritoneal Dialysis – KES 85,200 per month
• Pre-transplant recipient evaluation – Limit of KES. 150,000 per household
• Recipient surgery – KES 700,000
• Donor nephrectomy – KES 168,000
• Post-renal replacement therapy – Limit of KES 200,000 per household
Medical Imaging
• MRI – KES 11,000
• Mammography – KES 3,000
• CT Scans – KES 6,900
• Fluoroscopy – KES 4,000
• CT Angio – KES 8,000
• Echocardiograms (ECHO) – KES 3,500
• Specialized ultrasounds (Dopplers) – KES 5,000
• Electroencephalograms (EEGs) – KES 8,000 for a child and KES 5,000 for an adult.
• 2 per household per annum
Surgical Package
• Minor Surgery up to KES 145,600
• Major Surgery up to KES 280,000
• Specialized Surgery up to KES 1,120,000
Outpatient
• Essential diagnostic laboratory investigations for Diabetes, Hypertension, Sickle-cell & COPD/Asthma(once per person per annum)
Diabetes – KES 4,300
Sickle cell – KES 6,800
Hypertension – KES 2,850
COPD/Asthma – KES 700
Overseas Treatment
KES 500,000
Mental Wellness
Drug & Substance Abuse Rehabilitation – KES 67,200
Critical Care Services – ICU/HDU
KES 28,000 per day of admission up to 12 days
Oncology
KES 150,000 per beneficiary
Accident & Emergency
Up to KES 107,633
Ambulance Services
Intra Metro (25 km Radius) – KES 4,500
> 25 km – KES 75 per km
Interplay between the additional Package and POMSF Benefits
SHIF: Public officers are enrolled in SHIF like all employed Kenyans, but POMSF shall acts as a top-up scheme. When SHIF benefits are exhausted (e.g., hospital bills exceeding SHIF cover), POMSF steps in to provide additional protection for civil servants and their dependents.
ECCIF Role: Government-funded; provides coverage for emergency, chronic, and catastrophic illnesses (e.g., accident & emergency, cancer treatment, ICU/HDU). Accessible to all Kenyans. Public officers benefit from ECCIF first, like all citizens, for life-threatening conditions. POMSF bridges any financing gaps not fully covered by ECCIF, ensuring public officers and their dependents have full access to advanced treatment.
PHCF Role: Provides basic outpatient and promotive health services at the primary level, fully funded by government. Accessible to all Kenyans registered under SHA. POMSF only supplements by covering enhanced or specialized services once basic care pathways are exhausted



